
Low humidity and its effects
on airborne infection
Everyone releases tiny water droplets, called aerosols, when they breath, talk, cough or sneeze. The microscopic droplets contained in these aerosols are composed of around 97% water and 3% solutes - salts, proteins and numerous other substances.
Under normal circumstance, this personal contribution to the "air we share" has no negative effect on us. However, when a person has respiratory viral or bacterial infection, their exhaled air will contain harmful, contagious microbes. Once emitted into the air, these harmful microbes can infect other people, either by direct inhalation or through deposition on to a surface and subsequent touch contact.
The humidity of air is a major factor in the transmission of airborne microbes.
In dry atmospheres below 40%RH expelled droplets rapidly lose their moisture content through evaporation. As smaller droplets remain airborne for longer, this evaporation results in more droplets capable of staying airborne and increases the overall time they can float around for.
The droplet's water loss also changes its structure to a crystallized solid state. Viruses and bacteria get preserved in a floating capsule, where they remain infectious and have a greater potential to infect other people.
In an atmosphere above 40%RH, expelled droplets retain their moisture content, are heavier and less able to remain airborne. Furthermore, the dissolved salts inside the remaining airborne droplets create a hostile environment for any suspended microbes, decreasing their infectious nature and any risk they pose to health.
A humidity above 40%RH combats airborne infection by reducing the quantity of microbes in the air and inhibiting their infectious capability.

Droplets less than 4 microns expelled during breathing, speaking, coughing or sneezing can remain airborne and infectious for hours.

In humidity above 40% supersaturated solutes in the infectious aerosols inactivate the microbes and protect us from infections. The water containing droplets settle faster and have shorter "floating time" than in lower humidity atmospheres.
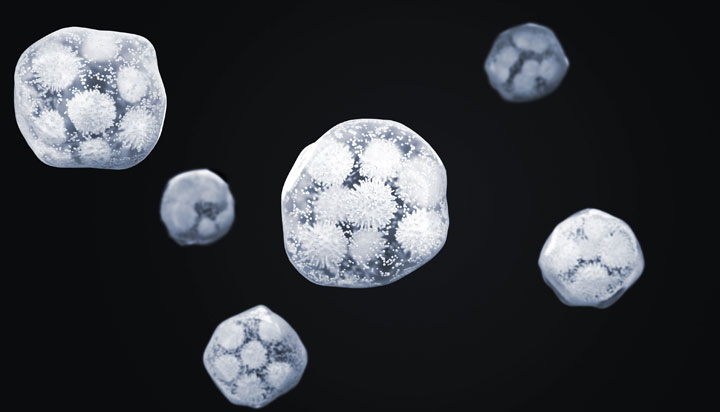
Below 40%RH infectious droplets lose their water content and become “dry aerosols”. Microbes get incorporated in the dry structures of the solutes, are preserved and remain infectious for longer. "Floating time" and the number of microbes is increased, compared to atmospheres with a humidity greater than 40%RH.
Parhizkar et al 2022
This study set out to examine the effects different environmental control strategies had on COVID viral load suspended in the air, with a view to rec...
Read moreJennifer M. Reiman et al 2018
This study set out to discover whether humidification of classroom environments during winter could reduce influenza virus survival and transmission.
Read moreDietz L. et al 2020
This literature review's aim was to provide actionable and achieveable guidance to built environment decision makers attempting to minimize infectiou...
Read moreCasanova LM et al 2010
Analysis of the survival and inactivation of coronavirus on surfaces at different temperature and humidities.
Read moreKoep T et al 2013
Study of the viability of raising the humidity in classrooms through humidification to a level that would reduce the airborne survival rates of flu.
Read moreAlsmo T, Alsmo C 2016
Comparison of the humidity levels in two office buildings, one with natural ventilation and the other with mechanical ventilation.
Read moreYang W et al 2012
Examination of the viability of flu in droplets containing different solutes at varying humidity levels, to isolate their effects on the virus.
Read moreDunklin EW, Puck TT 1948
Examined the decay rate of airborne bacteria at varying humidity levels and in different suspension solutions
Read moreShaman J et al 2010
Review of studies to explore the relationship between absolute humidity levels of air and airborne 'flu transmission and virus survival times.
Read moreMyatt TA et al 2010
Modeling analysis of the effect of a humidifier in a domestic environment and its impact on the survival of airborne influenza A virus.
Read more